Researchers at McMaster University have solved a vexing problem by engineering surface coatings that can repel everything, such as bacteria, viruses and living cells, but can be modified to permit beneficial exceptions.
The discovery holds significant promise for medical and other applications, making it possible for implants such as vascular grafts, replacement heart valves and artificial joints to bond to the body without risk of infection or blood clotting.
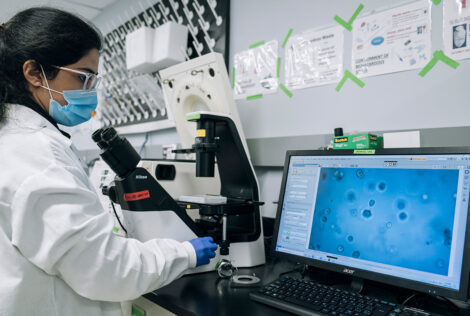
The new nanotechnology has the potential to greatly reduce false positives and negatives in medical tests by eliminating interference from non-target elements in blood and urine.
The research adds significant utility to completely repellent surfaces that have existed since 2011. Those surface coatings are useful for waterproofing phones and windshields, and repelling bacteria from food-preparation areas, for example, but have offered limited utility in medical applications where specific beneficial binding is required.
“It was a huge achievement to have completely repellent surfaces, but to maximize the benefits of such surfaces, we needed to create a selective door that would allow beneficial elements to bond with those surfaces,” explains Tohid Didar of McMaster’s Department of Mechanical Engineering and School of Biomedical Engineering, the senior author of a paper that appears today in the journal ACS Nano.
In the case of a synthetic heart valve, for example, a repellent coating can prevent blood cells from sticking and forming clots, making it much safer.
“A coating that repels blood cells could potentially eliminate the need for medicines such as warfarin that are used after implants to cut the risk of clots,” says one of the lead co-authors Sara Imani, a McMaster PhD student in Biomedical Engineering.
Still, she explains, a completely repellent coating also prevents the body from integrating the new valve into the tissue of the heart itself.
By designing the surface to permit adhesion only with heart tissue cells, the researchers are making it possible for the body to integrate the new valve naturally, avoiding the complications of rejection. The same would be true for other implants, such as artificial joints and stents used to open blood vessels.
“If you want a device to perform better and not be rejected by the body, this is what you need to do,” says lead co-author Maryam Badv, also a McMaster PhD student in Biomedical Engineering. “It is a huge problem in medicine.”
Outside the body, selectively designed repellent surfaces could make diagnostic tests much more accurate by allowing only the particular target of a test – a virus, bacterium or cancer cell, for example – to stick to the biosensor that is looking for it, a critical advantage given the challenges of testing in complex fluids such as blood and urine.
The researchers, who collaborated with Dr. Jeffrey Weitz of the Thrombosis & Atherosclerosis Research Institute at Hamilton Health Sciences to understand the challenges related to making successful implants, are now working on the next stages of research to get their work into clinical use.